IVC Assessment for Fluid Responsiveness
- Position the patient supine.
- Obtain a subxyphoid view of the heart.
The ultrasound indicator should be directed toward the patient’s left flank.
- Once you have identified the right atrium, turn the ultrasound probe 90 degrees counterclockwise.
The indicator should now be directed toward the patient’s head.
- Identify the IVC as it enters the right atrium.
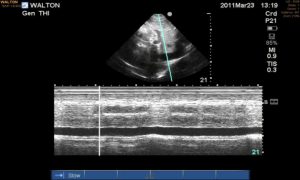
- Put the ultrasound into M-mode.
- Place the M-mode cursor cross the IVC approximately 2 cm inferior to the junction with the RA.
- In spontaneously breathing patients, the following measurements suggest a patient is likely to be fluid responsive:
- IVC measuring < 1 cm in diameter coupled with IVC collapse > 50% with each breath or
- IVC collapsibility > 42%
IVC collapsibility = (max diameter – min diameter) / (mean diameter) x 100
- In mechanically ventilated patients who are passive on the vent, fluid responsiveness is likely if the IVC distensibility > 18%.
IVC distensibility = (max diameter – min diameter) / (min diameter) x 100
Barbier C, Loubières Y, Schmit C, Hayon J, Ricôme JL, Jardin F, et al. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med. 2004;30(9):1740–6.
Airapetian N, Maizel J, Alvamani O et al. Does inferior vena cava respiratory variability predict fluid responsiveness in spontaneously breathing patients? Critical Care. 2015;19:400.