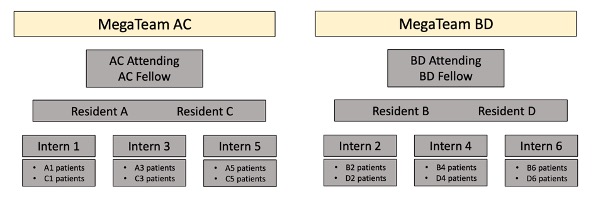
Overall structure
There are 2 MegaTeams (A/C and B/D), each with 2 Residents and 3 Interns. Each MegaTeam will round as a group and the Senior Residents on the team should be familiar with all of the teams’ patients (and able to support all 3 Interns for all patients on the MegaTeam. Patients will be categorized according to the Resident & Intern who admitted them (i.e. PAR score for a patient would be A1 if they were admitted by Resident A & Intern 1).
Every day, there will be one team with a Senior Resident On-Call (28 hour call, admitting 6:00am-6:00am with assistance from Night Float starting at 7:30 pm), one Long-Call Intern (admitting 6:00am-7:00 PM), and one Short-Call Intern (6:00am-5:00pm). They will all work together to alternate admissions throughout the day.
Overview of Call Structure:
Senior Residents:
Day 1: On-Call
Day 2: Post-Call
Day 3: Regular
Day 4: Pre-Call or Off
Interns:
Day 1: Long-Call
Day 2: Post-Long Call
Day 3: Regular day or Off
Day 4: Regular day
Day 5: Short-Call
Day 6: Post-Short Call
Night Team: There is one night team with 1 Night Float Resident and 1 Night Float Intern.
- The NF Resident will be off Friday night (covered by MICU ESP shift)
- NF Intern will be off Sunday night. NF resident admits alone
Bridge Resident: There is one Resident who serves as a “Bridge” Resident (2:00pm-12:00 AM M-F, 12:00pm-12:00 AM weekends). Bridge takes cross-cover from non-call teams and helps support the unit in general (supports interns who need help, procedures, helps with admissions if the call resident is very busy). Bridge day off is Tuesday (call resident’s sister-senior takes cross cover)
Call Day Structure
- By 6AM at the latest: teams arrive and take signout/pagers from the NF intern. Call resident signs into admitting pager (p6428). Post-call / NF resident discuss which case will be teaching case with call fellow
- ~6:40AM: interns touch base with seniors about patient plans
- 7AM: both MegaTeams join together for teaching case. Triage and Dayfloat are present.
- 7:15AM: MegaTeams split and round. NF team presents first, followed by all of post-call resident’s patients.
- ~9AM: Post-call resident should complete rounding. Post-call resident +/- post-call interns, APNs, ED dayfloat run the list of tasks prior to post-call resident leaving
- BY 10AM: Post-call resident should leave the hospital.
- 10AM: Pulm/CC Morning Report if time allows (tenth floor CCD)
- 2PM-3PM: MICU Lecture for all residents and interns (in MICU workroom)
- 3PM: PM rounds with attendings, fellows, call resident, and bridge resident. Fellows present, bridge resident records relevant PM plan in epic where able to also be accessed by NF
- 4PM: Teams can begin to sign out to Bridge Resident (or, if Tuesday, to the sister to call resident). ED dayfloat may leave if the post-call team work is done
- 5PM: Short call intern stops admitting patients
- 7PM: Long call intern stops admitting patients
- 7:30PM: NF resident and intern arrive. NF resident signs into admitting pager. If Tuesday, night team takes sign-out from the call resident sister senior
- 8PM: Short call intern should leave by 8PM at the latest
- 9:30PM: Long call intern should leave by 9:30PM at the latest
- 10:30PM: Bridge Resident begins signing out to NF Resident and NF Intern. On slow nights, this sign-out can occur earlier (especially since sign-outs often get disrupted), but Bridge should remain FCP on cross-cover patients until midnight.
- 12AM: NF intern signs into cross cover pagers. Bridge resident leaves.
Overnight Admissions & Redistribution
- Fill the post call teams first, up to a cap of 7 patients per Intern. Prioritize filling the post long call intern, followed by the post short call intern
- When the post call team is capped, additional patients can be given to the non post call intern at the discretion of the Fellows ONLY if that intern’s other senior is working that day
- Additional patients can be distributed to the call team, with preference given to late admits (from NF) or highly active patients, all at the discretion of the fellows
Rounding Order
- Teaching case (weekdays only; designated in discussion with the call resident, NF resident, and fellow)
- Night Team presents to Post-Call MegaTeam
- If applicable, Night Team then presents overflow admits to the other (On-Call) MegaTeam
- Post-Call Team presents their news and olds (i.e. if Resident A is post-call, all of the “A” patients will be presented at this time, followed by all of the C patients afterwards).
- The On-Call MegaTeam will round geographically as a group.
Intern’s guides to the MICU
- See Intern’s Guide to the MICU which contains high-yield knowledge written by the attendings for the interns
MICU Orientation Guide
MICU Evaluations and Admissions:
- Any patient who cannot be appropriately managed by a floor team will be considered suitable for ICU admission. Just because a patient does not meet a “strict” indication for MICU admission does not mean they don’t need to come. Patients whose care is limited by floor nursing or RT ratios may be appropriate transfer to the MICU.
- All consults should be run by the fellow, particularly if not admitting to the MICU. Some non-medicine services routinely admit patients to the MICU: ENT, orthopedics, obstetrics/gynecology, and urology all admit their critically ill patients to the MICU rather than another ICU.
- All residents evaluating a patient for transfer must write a MICU evaluation note. All evaluations should be discussed with the MICU fellow. Evaluation notes should provide recommendations for management and anticipatory guidance when the patient is not being accepted to the MICU
- Patients whose clinical condition and evaluation are primarily of a cardiac nature should be managed in the CCU. However, such patients who have excessive co-morbidities may be admitted to the MICU. The CCU and MICU fellows should be involved in these triage decisions
- Between 10 pm and 6 am, OSH transfers will only be able to come to beds on 9N, 9S, and 8S. When the MICU is very busy, the call resident should discuss stopping all OSH transfers with the MICU fellow. If approved, the Fellow should contact the transfer center to relay this message.
Transferring Patients out of the MICU
- MICU decides the patient is appropriate for floor transfer and pages 9100 (hospitalist triage) before writing the transfer order. If 9100 has not responded to you within 15 minutes, you may page again.
- 9100 will call back and assign the patient to a receiving team. You can place the transfer order to the location they instruct you. They will pass your information along to the admitting team to call you for signout.
- Transfer note and transfer order reconciliation should be completed prior to transfer.
- Careful communication and signout are essential as clinical stability of MICU patients can change abruptly.
- Once verbal signout is given, the patient’s FCP can be changed. The receiving floor team can assume responsibility for the patient 24/7, even if the patient is still physically located in the ICU. However, the patient will remain on the MICU Master List until they are physically transferred out of the unit and should be included in cross-cover signout (so that the covering resident is familiar with the patient if they are pulled into the room by a MICU nurse for an urgent issue). The floor team will remain the primary caregiver and receive all FCP pages. Patients will be removed from the Master List once they are physically transferred out of the unit.
- If a patient is transferring late (after dayteam signout), it is essential the transfer note is thorough and up to date. The bridge or night float resident will use it to give the admitting team signout. The next morning, the day team can reach out to the admitting team to close the loop of communication and answer any remaining questions.
End of Service and Day Off Signout
- Signout emails at the end of your service should always be sent to both the oncoming team member you are signing out to and the intern/resident remaining on service when you leave.
- Signout emails should be provided if you will be off and your intern or resident was not present the day before (e.g. you are the intern and you will be off tomorrow. The resident was post-call during the day and will be resinterning of your patients the following day).
Overview of MICU Resident Roles
Long call intern
- 6AM – 7PM: Admit patients with the call resident
- 7PM-9PM: Wrap up plans and notes for new admits
- 9:30PM: Leave hospital at the latest
- Cap: 5 H&Ps, 7 patients total
Short call intern
- 6AM-5PM: Admit patients with the call resident
- 5PM-8PM: Wrap up plans and notes for new admits
- 8PM: Leave hospital at the latest
- Cap: 5 H&Ps, 7 patients total
Call resident
- 6AM-7:30PM: Cover admitting pager. Triage and admit patients. Help NF admit after 7:30 if busy. Discuss all evaluations with the fellow.
- 3PM-4PM: Attend PM rounds
- 7:30-9:30 PM: Help interns with plans and notes to ensure they leave the hospital on time.
- 9:30PM-6AM: Continue to care for new admits, help NF with admissions or cross-cover
Bridge resident
- Weekdays: 2PM – 12AM
- Weekends: 12PM – 12AM
- Off Tuesdays – on these days the sister to call resident will take signout until 7:30PM, and give signout to the NF team when they arrive at 7:30PM
- Primary role is cross-cover, but should also help with other tasks needed by the unit (procedures, help with getting interns out on time)
- Weekends: Start taking cross-cover at 12PM. No PM rounds or lecture. Otherwise same as weekdays, seen below:
- 2PM: Attend MICU lecture
- 3-4PM: Attend PM rounds. Take notes on patients in epic where accessible by NF resident.
- 4PM onwards: Take signout from non-call residents. Help call and NF residents
- 10:30PM: Start signing out cross-cover to NF team
- 12AM: NF intern signs into cross-cover pagers. Bridge resident leaves
Night float (NF) resident
- 7:30PM: sign into admitting pager, admit patients. Utilize bridge and call resident as needed when busy
- 10:30PM: Begin hearing signout from bridge resident
- 12AM: aid NF intern in cross-covering patients
- 7AM: aid NF intern in presenting overnight patients on rounds
- Off Fridays: covered by MICU ESP provider
Night float (NF) intern
- 7:30PM: Admit with the NF resident
- 10:30PM: Begin hearing signout from bridge resident
- 12AM: Take over cross cover pagers from bridge resident
- 7AM: Present overnight admissions on rounds
- Cap: No more than 5H&Ps per night
- Day off: Sunday (on this night, NF resident admits alone)
ED Dayfloat
- Role is to help the post-call megateam: both post-call resident patients as well as those interns other patients. On most post-call days, both seniors will not be present, so the ED dayfloat will help interns complete their tasks and advance care
- On blocks with only one ED dayfloat assigned, days off will be Mon/Thurs, unless a day off has been moved to allow for ED dayfloat presence on days where no APNs will be present
- On blocks with two ED dayfloats assigned, at least one ED dayfloat will be present every day of the block (1 week on/ 1 week off)
- 7AM: Arrive. Attend rounds for post-call megateam
- Weekdays: help interns advance care until at least 4PM or the work is done, whichever is later
- Weekends: help interns advance care until at least 12PM or the work is done, whichever is later
- Responsibilities:
- Assist interns with all patient care
- Write transfer summaries
- Update signouts
- Supervise interns with procedures if the dayfloat is proficient and signed off on procedures
- Help transport unstable patients
- Assist the call team if the post-call team does not require additional assistance
APNs
- Weekdays: 7:00am – 7:00pm (with some exceptions)
- Weekends: 7:00am – 1:00pm (with some exceptions)
- Responsibilities:
- Primarily aid in advancing care for post-call patients (including orders, consults, family meetings, procedures)
- Can assist call team if post-call team does not require additional assistance
Updated 6/2025